Cushing’s Syndrome in Children
- The incidence of endogenous Cushing’s syndrome is approximately 2 to 5 new cases per million people per year, and approximately 10% of these new cases occur in children.
- The most common cause of endogenous Cushing’s syndrome in children is an ACTH-secreting pituitary adenoma (accounts for approximately 75% of all cases of endogenous Cushing’s syndrome in children older than 7 years)
- The most common cause of Cushing’s syndrome in infants and toddlers is an adrenal tumor (adenoma, carcinoma, or bilateral hyperplasia).
- Bilateral nodular adrenal disease is an ACTH-independent cause of Cushing’s syndrome. Children and adolescents with bilateral nodular adrenal disease may have periodic or “cyclic” Cushing’s syndrome. Bilateral nodular adrenal disease may be associated with genetic disorders such as Carney’s complex or McCune Albright Syndrome.
Symptoms & Signs of Cushing’s in Children
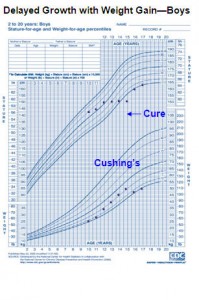
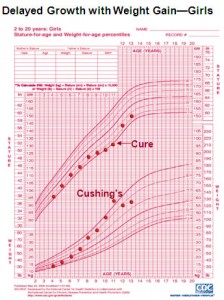
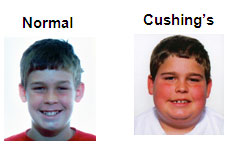 In many children the onset of Cushing’s syndrome may be insidious. Growth failure (or deceleration) associated with weight gain is a hallmark feature of Cushing’s syndrome in children. Other sign and symptoms often seen in children and adolescents with Cushing’s syndrome include facial plethora, increased fine downy hair on the face, body and extremities, a temporal fat pad, round face, diabetes and other symptoms listed below.
In many children the onset of Cushing’s syndrome may be insidious. Growth failure (or deceleration) associated with weight gain is a hallmark feature of Cushing’s syndrome in children. Other sign and symptoms often seen in children and adolescents with Cushing’s syndrome include facial plethora, increased fine downy hair on the face, body and extremities, a temporal fat pad, round face, diabetes and other symptoms listed below.

| Presenting Symptoms & Signs of Cushing’s Syndrome | |
| Symptom | Frequency % |
| Weight Gain | 90 |
| Growth Retardation | 83 |
| Menstrual Irregularities | 81 |
| Hirsuitism | 81 |
| Obesity (BMI > 85th percentile) | 73 |
| Violaceous skin striae | 63 |
| Acne | 52 |
| Hypertension | 51 |
| Fatigue-weakness | 45 |
| Precocious puberty | 41 |
| Bruising | 27 |
| Mental Changes | 18 |
| “Delayed” bone age | 14 |
| Hyperpigmentation | 13 |
| Muscle weakness | 13 |
| Acanthosis nigricans | 10 |
| “Accelerated” bone age | 10 |
| Sleep disturbances | 7 |
| Pubertal Delay | 7 |
| Hypercalcemia | 6 |
| Alkalosis | 6 |
| Hypokalemia | 2 |
| Slipped femoral capital epephysis | 2 |
| Adapted from Magiakou M, Mastorakos G, Oldfield EH, et al, Cushing’s Syndrome in Children and Adolescents. Presentation, Diagnosis, and Therapy. (New England Journal of Medicine, 1994: vol. 331 no. 10, p 629-636)</td> | |
Testing
- It is important for children to be evaluated by a pediatric Endocrinologist who is experienced with Cushing’s Syndrome, since some tests require adjustment for the child’s size.
- The best screening test for Cushing’s Syndrome in children is a collection for urinary free cortisol (UFC). The results must be adjusted for the child’s size.
- Diurnal cortisol: Normally, the cortisol level is very low at midnight, but with Cushing’s Sydrome, the midnight are levels are usually higher than expected; often not very different from the early AM cortisol. Diurnal cortisol measurements can be obtained by blood draws or salivary cortisol (1) measurements collected at 7:30-8:00 AM and 11:30-12 PM. The FDA recently approved a salivary cortisol assay (2) however this this test has not been validated in children. The FDA approved assay is available from ACL Labs (800-877-7016), Salimetrics (800-790-2258), or Esoterix (800-444-9111).
- Low-dose dexamethasone test: This test involves giving one milligram of dexamethasone (adjusted for the child’s weight) and measuring the AM cortisol level in blood. The low-dose dexamethasone test has not been validated extensively in children, but results of a study done at N.I.H. show that AM cortisol should be less than 5mcg/dL.
References
- Gafni RI, Papanicolaou DA, Nieman LK Nighttime salivary cortisol measurement as a simple, non-invasive outpatient screeing test for Cushing’s syndrome in children and adolescents. J. Pediatr. 2000 July 137(1):30-35.
- Raff H, Homar PJ, Skoner DP. New enzyme immunoassy for salivary cortisol (Letter) Clin Chem. 2002;48:207-8.
Growth Charts: Courtesy of N.I.H.
Photos: Courtesy of CSRF Fall, 2004
Printed by: The Cushing’s Support and Research Foundation
65 E. India Row #22B
Boston, MA
website: http://CSRF.net
email: [email protected]



