The Experience of Chronic Illness
If you have ever felt like no one in your life can truly comprehend what it’s like to survive through the experience of Cushing’s, maybe it can be a small bit of comfort that virtually 100% of patients report some level of misunderstanding, ignorance, and even intolerance from friends, family, and co-workers. Sometimes there are one or two curious people in your circle who take the time to research the disease, but for the most part it seems like the enormity of what’s happening inside us is lost on most audiences. Conversely, our loved ones’ protective intentions can also lead to suffocating and coddling behavior “for our safety”.
For many of us, managing how a chronic illness fits into our lives becomes a piece of the puzzle to juggle after treatment. Living with an invisible illness is frustrating and isolating, but in some cases it can lead to depression, significantly reduced quality of life, and other situations where patients might need to be their own advocate – again! – to make sure their mental health is prioritized.
Dr. JoAnn LeMaistre is a psychotherapist and speaker who learned she had Multiple Sclerosis at a pivotal point in her life – she had just had a baby and gotten her PhD in clinical psychology. She wrote a book called After the Diagnosis: From Crisis to Personal Renewal for Patients with Chronic Illness. This amazing quote comes from her book:
“Central to wellness is the concept of adaptation — the flexible, creative use of resources to maximize your choices and experiences of mastery. This is the key to creating and sustaining a sense of inner tranquility in the face of difficult realities. There is no need to deny grim facts of existence or to pretend to others that all is well when inside there is little except torment. To be psychologically well while physically sick involves the belief that your personal worth transcends physical limitations; you need positive self-esteem for true adaptation. This belief in your self-worth rarely emerges until what you have lost and grieved for stands second in importance to precious moments of inner peace and joy.”
In After the Diagnosis, Dr. LeMaistre summarizes six stages of normal emotional reactions when a chronic illness like Cushing’s becomes a part of your life. They can come in any order, they often repeat, and not everyone goes through each one. Family support and the patient’s mental state, flexibility, personality, stress tolerance, and other characteristics play roles in how each stage is experienced.
- CRISIS – The patient is seriously ill, scared, and consumed with the emergency of the illness. Those around the patient usually have no problem understanding what is happening because it is the focus of everyone’s attention. Survival is the #1 goal and most things are muted in favor of hyperfocus on the patient. No one knows what’s going to happen.
- ISOLATION – The illness has settled in and the initial crisis has probably calmed down a bit. Everyone’s starting to comprehend that this is going to be around for a long time. The patient is frequently depressed and anxious about their new dark passenger. Family and friends are also exhausted at this point.
- ANGER – The most dangerous stage has the patient usually blaming themselves for the illness that is disrupting everyone’s lives. The worst possible outcome of this stage is suicide. The patient sees themself, not the illness, as the cause of the problems. There is heavy strain on the family.
- RECONSTRUCTION – The patient is better or is successfully using adaptive skills. Time is no longer frozen and everyone can look to the future with the “new normal”. The most important element of life to be reconstructed is our emotional state.
- INTERMITTENT DEPRESSION – Dr. LeMaistre describes the “phantom psyche” that shows up and causes you to think if only you didn’t have this disease, you could be doing things as you did before. It presents unrealistic expectations. Outwardly, what to us feels like introspection is frequently misread as self-pity. Anniversaries trigger memories and sadness.
- RENEWAL – No longer focused solely on adjusting and adapting, this is an opportunity to look at what we CAN do, and start doing it.
Alpine Guild, publisher of Dr. LeMaistre’s book, offers an extended excerpt on their website from After the Diagnosis that goes into much more detail than this. We highly recommend you read it to get the full impact of her wisdom on this subject. Find it at alpineguild.com/COPING WITH CHRONIC ILLNESS.html (must capitalize the second half of the web address, and the spaces between the words are intentional and are not dashes or underscores).
Coping with a Chronic Illness
Dr. Ann Steiner, psychotherapist, is another expert on this topic. She presented at a Cushing’s Awareness Patient Day several years ago and shared resources about depression and coping. Dr. Steiner thinks it’s important to consider the family messages we got when we were growing up that shaped the way we conduct ourselves as adults. Are we conditioned not to ask for help even when we need it, for fear of imposing or being ridiculed? Was complaining met with help and comfort, or ignored? What subtle signs did we receive about being a burden? What ethnic or religious traditions encouraged or stifled other types of expression?
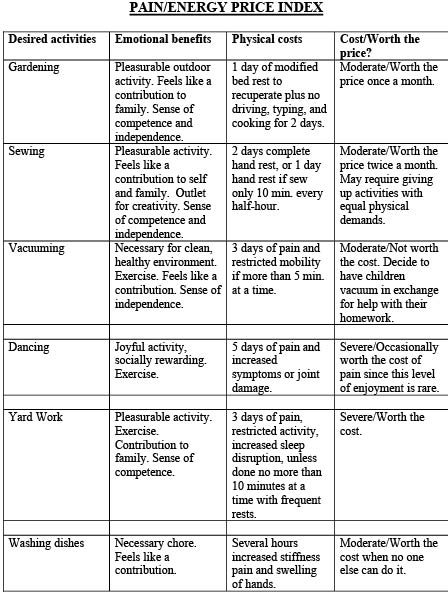
She also advocates for considering what she calls the Pain / Energy Price Index when deciding whether or not to do desired activities that are affected by the illness. The following chart uses some common activities as examples of times when a person with a chronic illness might have to leverage available energy and accommodate inevitable after-effects.
We are lucky to have caught Dr. Steiner’s ear for a few questions:
Q: There is research that points to significant rates of new depression and worsened existing emotional/mental conditions post-surgery in our community, and yet psychological wellness doesn’t seem to be a major part of the care plan for most patients. It can be really difficult to be proactive when you’re experiencing depression. Any tips on good ways to get past the self-barricade to seek help?
A: This is such an important question! Too often doctors and families focus on the medical issues, and don’t know how to address the emotional effects of the medical issues. Remember the phrase “psychosomatic” – often used to discount one’s medical reality? I prefer to think in terms of having any chronic medical condition as somatopsychic. In other words, if you have a medical condition, heart problem, etc., there are inevitable emotional side effects that are important to acknowledge. I think about living with chronic illness or pain as living over an underground river of sadness, or grief. Most of the time the losses and sadness are underground. When set-backs, flares, or new medical issues arise, or other stresses, losses and traumas happen, those emotions lurking underground may surge up and be disturbing. It can help to know that there will be times when you lose your emotional equilibrium. If therapy, journaling or other coping tools aren’t in your toolkit, consider talking to a trusted friend so you don’t have to be alone during challenging times.
Q: You warn of the misuse and abuse of “positive thinking” and the power of words. Can you explain further?
A: While it is important in many ways to be positive and to invest in self-care, too often well-intentioned comments from loved ones can, unintentionally, be hurtful. For example, if someone says, “You just need to try harder,” you are likely to feel blamed for having the illness. Barbara Ehrenreich addresses the downsides of positive thinking in her important, provocative book, Bright-sided: How the Relentless Promotion of Positive Thinking Has Undermined America.
Q: The poem you quote on your website, “Choice + Chance = Change”, is a powerful way of seeing self-help and self-advocacy, but not everyone can look at it and imagine enacting it for themselves. Is it ok to allow oneself to stay in a low for a period of time when the effort to do the opposite feels like it’s doing more harm than good?
A: Definitely! As Dr. LeMaistre so beautifully describes, intermittent depression is a normal response to a chronic condition. Set-backs, flares, and other life stresses and losses are all times that are likely to create more depression. Feeling depressed, while normal at times, can be made less painful by talking about it with a psychotherapist, a clergyperson, in a group, with trusted friends, or through freewriting. Exercise, as appropriate for you, has been shown to help with depression, as has mindfulness meditation. Finding ways to make room in your life for the rollercoaster of your chronic condition, without being defined by your medical diagnosis, is a large, yet important project.
Q: Any warning signs to look for that the stay is starting to be too long?
A: Depression can interfere with normal functioning – in relationships, work, and family life. Without help, it can lead to thoughts of hurting oneself or others. Thoughts and comments about not wanting to live need to be taken seriously, not discounted as “just trying to get attention.” Instead, most often such comments mean that the person is in significant emotional pain and needs professional help. As the American Psychological Association’s Help Center (apa.org/topics/depression/index.aspx) says, “Depression is more than just sadness. People with depression may experience a lack of interest and pleasure in daily activities, significant weight loss or gain, insomnia or excessive sleeping, lack of energy, inability to concentrate, feelings of worthlessness or excessive guilt and recurrent thoughts of death or suicide.” Withdrawal, persistent, intense feelings of sadness, and noticeable changes in motivation are warning signs of depression.
Another important warning sign is if you become obsessed with negative thoughts. If they persist, it is important to tell your physician(s), especially since, as I mention in the depression checklist that follows, depression can be a side effect of medications and can become life-threatening. Some research indicates that pathways in the brain get created if clinical depression goes untreated for more than six weeks. If you aren’t getting any breaks in feeling depressed, if you get stuck in feeling that all you are is your disease, those are times when it is best to get professional help.
I remember being impressed by a candid radio interview with Maya Angelou who famously said, “I’ve learned that no matter what happens, or how bad it seems today, life does go on, and it will be better tomorrow.” In that interview she mentioned considering suicide and being told that she could always chose to end her life another day, but that if she made that decision on that day she wouldn’t be here to see how things got better in days ahead. She spoke of her gratitude for having chosen life at a time when she felt she had lost all hope.
As a reminder, The National Suicide Prevention Lifeline can be reached at 1-800-273-8255 or online at suicidepreventionlifeline.org. Their online chat at suicidepreventionlifeline.org/chat is worth having easy access to.
Q: We’ve lost fellow Cushing’s patients to suicide this year. Your lists of symptoms of and facts about depression are at the end of this article, but are there any things we can be alert to in other people who may be suffering and need help? It’s hard to see through a great actor‘s or actress’ façade of wellness, but there must be clues. We need to look out for each other too.
A: First, please accept my deepest condolences to you and your community! Since there are times
when it helps to pretend to be fine, it can become easy to “pass” and hide one’s emotional pain. One side effect of depression is that it gets in the way of thinking clearly. Feeling hopeless and concerns about being a burden can increase feelings of worthlessness that feed suicidal thoughts. I address some of these issues in my article, “Tool Kit for Families Living with Chronic Medical Illness” (drsteiner.com/artpub_articles_toolkitfamilies.html). About how you can look out for each other, that is a big question, worth more attention than just a few sentences here can address. Having a therapist give a talk about this important topic, and/or write an article about it, is worth considering. For now, consider talking with each other about your feelings and beliefs about suicide, and make one-on-one agreements with each other that if things get that bad that you will let each other know, and reach out for help. Two resources worth having easy access to are:
– Befrienders Worldwide, an organization of providers of emotional support and suicide prevention (befrienders.org)
-The National Suicide Prevention Lifeline, contacts earlier in the article, “provides free and confidential emotional support to people in suicidal crisis or emotional distress 24 hours a day, 7 days a week, across the United States. The Lifeline is comprised of a national network of over 150 local crisis centers, combining custom local care and resources with national standards and best practices.”
Q: What are you working on right now?
A: I will be revising the Pain/Energy Price Index for The Rollercoaster of Chronic Illness: How to Add Joy to the Ride, have a chapter about the Art of Complaining Without Clearing the Room, and am expanding the section currently on my website about nicknaming your illness. I would love to have your readers make suggestions for examples of activities they enjoy which are costly physically for the revision of the Pain/Energy Price Index, and have them be beta readers when the book is ready.
Symptoms of Depression
- Feelings of extreme sadness or despair for at least two weeks or longer
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness, pessimism
- Increased use of drugs and/or alcohol
- Social withdrawal, isolation
- Major change in self esteem, deterioration in hygiene habits
- Feelings of guilt, self-condemnation
- Anger, worthlessness, helplessness
- Loss of interest or pleasure in hobbies and activities that were once enjoyed, including sex
- Decreased energy, fatigue, being “slowed down”
- Difficulty concentrating, remembering, making simple decisions
- Insomnia, early-morning awakening, or oversleeping
- Appetite and/or weight loss or overeating and weight gain, not medication related
- Thoughts of death or suicide, talk of harming self or others, suicide attempts
- Restlessness, irritability
Facts About Depression
- Depressed individuals tend to feel helpless and hopeless and to blame themselves for having these feelings. This cycle often interferes with asking for help.
- There are many forms of depression. Some people experience a few symptoms, some many. Severity of symptoms varies with individuals and also varies over time.
- People who are depressed may become overwhelmed and exhausted and stop participating in certain everyday activities altogether. They may withdraw from family and friends and have difficulty with routine activities.
- Having one episode of depression greatly increases the risk of having another episode. Some research indicates that ongoing psychotherapy may lessen the chance of future episodes or reduce their intensity.
- Research has shown that the combination of psychotherapy and antidepressant medication reduces life-impairing problems of depression.
- Chronically ill patients are at higher risk for depressive reactions, hence it is important that they report changes in mood to their physicians.
Reminder: Depression can be a symptom of Cushing’s and a side effect of certain medications. Be sure to notify your physicians if you have significant mood changes.
Editor’s Note: Many thanks to Dr. Ann Steiner for her permission to use the Pain / Energy Price Index and to print the above Symptoms of and Facts About Depression. Please visit her website at DrSteiner.com for more resources, to share your input, or to contact her directly.




Sorry, comments are closed for this post.