Dr. Anthony Heaney, Co-Director of the UCLA Pituitary and Neuroendocrine Program and President of the International Pituitary Society, presented two sessions titled “What are the causes of adrenal insufficiency in adults and when do I need to stress dose?” and “What is Adrenal Crisis?” at the AIU conference. The following is my interpretation of these presentations and the accompanying slides.
Adrenal Function and Insufficiency
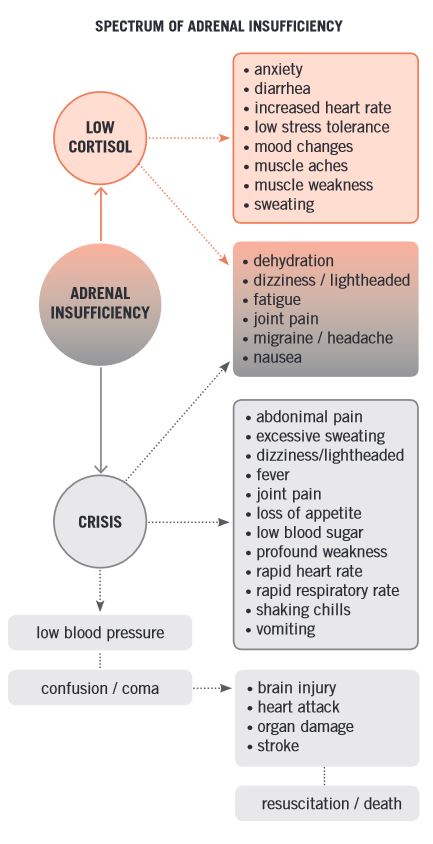
Knowing when to stress dose and what to do in an adrenal crisis are two of the most important questions that must be addressed when a patient enters adrenal insufficiency (AI). The patient is suddenly tasked with trying to adequately mimic the essential stress response that is unique to each of us with cortisol replacement while simultaneously becoming aware of conditions that can cause them to need more than just their maintenance dose to avoid becoming sick. Best case scenario has us quickly able to access our medicines at all times, but worse case sees an AI patient become very ill, unable to take oral medication, using an emergency injection, rushing to the ER, and/or worse.
It is helpful to think about stress as acute vs chronic. Our adrenal glands are built to handle both types of stress events, but that fact isn’t very useful if our adrenals are not working properly or have been removed. During acute stress, mechanisms in the brain send signals rapidly to nerves in the spinal cord that connect with the medulla (lowest part of the brainstem). This releases epinephrine (adrenaline) and norepinephrine. Within 30-40 seconds, heart rate and blood pressure go up, the liver produces glucose to deal with the event, and the lungs dilate.
Cortisol, metered and chronic in its approach, arrives on the scene when your brain anticipates an extended challenge. This entire process is mediated by hormones throughout your endocrine system. It causes retention of sodium and water in the kidneys, increases glucose production, and reduces insulin response to keep the glucose in the blood stream.
Dysfunction among the glands of the endocrine system impacts these processes. In primary AI, the adrenal itself is damaged. In secondary or tertiary AI, something else was damaged and caused problems in the adrenal.
In primary AI, there is an absence of cortisol and aldosterone, a hormone that regulates sodium and potassium. An example of primary AI is Addison’s Disease, which affects women and men equally at a ratio of about 1:100,000 people in the US. Symptoms of Addison’s can include extreme fatigue and weakness, salt craving, nausea and vomiting, low blood pressure and blood sugar, decreased appetite and weight loss, body hair loss, GI disturbances, and bronze pigmentation of the skin.
The origin of secondary AI frequently involves the pituitary – removal of an ACTH-secreting pituitary tumor or radiation to the pituitary, for example. There are other, less frequent causes including tuberculosis and gene mutations.
Treatment for AI depends on the type:
- Primary AI patients replace cortisol with hydrocortisone or cortisone acetate and replace aldosterone with fludrocortisone. Sometimes they replace androgens (testosterone or estrogen) with synthetic DHEA or Prasterone. If possible, it is optimal to treat the underlying cause of the AI.
- Patients with secondary AI brought about by damage to the pituitary replace cortisol with hydrocortisone or cortisone acetate. They sometimes replace other hormones such as thyroid, growth, and anti-diuretic. They do not have to replace aldosterone because their adrenals are intact and still performing this function which is not affected by the damage to the pituitary.
- Patients with steroid-induced AI are advised to work with their doctor to safely wean off the steroid, reduce intake of the steroid, and/or switch to a different medication.
For all patients with AI, it is important to work with your doctor to fine-tune your personal best dosage for daily maintenance and stress dosing. Your doctor needs input about your lifestyle so they can really understand you in your natural environment. Are you a couch potato or a marathon runner? Do you do better with two daily doses or a more personalized three or four? The challenge is to find the proper balance that keeps your cortisol from becoming too low but also protects against adverse effects of too much steroids: mood and sleep disturbances, weight gain, high blood pressure and blood sugar, osteoporosis, and other symptoms of high cortisol.
Stress Dosing
There is a spectrum of stress, and usually an adrenal crisis is brought about by more than just one thing. A catastrophic event could do it but more commonly it’s due to trauma or illness. It’s important to recognize the difference and not get into a situation where steroid doses are being increased too often, because that can lead to symptoms of hypercortisolism. There is always an exception to the rule – under certain circumstances of acute high stress, such as being placed into a situation of caring for a terminal parent, for example, short-term sustained increased dosing can help, but it’s extremely important to return to your normal dose as soon as possible. This highlights the value of helping your doctor determine the appropriate individualized dose for your life and what you’re experiencing.
Increasing hydrocortisone can present two types of effects: dose-dependent and duration-dependent. Dose-dependent effects are from large doses taken for short periods of time and can include temporary high blood sugar, psychosis and peptic ulcer disease. Duration-dependent effects appear when higher-than-needed doses are taken for long periods of time. Examples of this are high blood pressure, Cushingoid physical changes, frequent infections, and osteoporosis.
Osteoporosis is especially concerning because we only make bone until about age 22. That’s it for the rest of our lives. Bones don’t get better with time. It is recommended that we Cushing’s and AI patients have our bone density checked about every two years, preferably on the same machine. This can be challenging due to moving or insurance, but bone health should not be ignored.
Adrenal Crisis
We know our bodies best, but some of us are particularly good at giving the outward appearance that everything is ok when it’s not. AI and adrenal crisis do not have time for that nonsense. Prompt action is required to prevent dangerously low cortisol levels. Signs that you might be heading into an adrenal crisis include:
- fatigue, lack of energy, weight loss
- low blood pressure, dizziness, possible collapse
- abdominal pain, tenderness, nausea, vomiting
- fever
- confusion, sleepiness, in severe cases delirium or coma
- back and leg cramps and spasms
If you think you are heading into an adrenal crisis, hopefully you have rescue medicine and are trained and ready to give yourself an emergency injection of hydrocortisone if you cannot keep an oral rescue dose down. The next step is to be seen by or in touch with a doctor immediately. The life-threatening qualities of an adrenal crisis dictate that there are no adverse consequences to initiating life-saving treatment with hydrocortisone. Diagnostic measures should never delay swift treatment of a suspected adrenal crisis – they can be safely established once the patient is stable. Typically, after a patient is stabilized, they will continue to receive high doses of hydrocortisone and rapid rehydration for a short period of time, after which they will be tapered off the high doses with the guidance of their endocrinologist.
Putting it All Together
Managing AI is a delicate balance that requires control and attention to many moving parts. At the AIU conference, two things puzzled me in the beginning: it seemed like there were a lot of people who forgot to set their alarms to silent because they kept going off during the presentations, and everyone was very enthusiastic about the electrolyte samples being given out. I discovered that the alarms weren’t random – they were alerting that it was time to take a dose of hydrocortisone. The electrolytes address the lack of aldosterone in primary AI patients. One presenter had a box of broth with a straw sticking out – she called it her adult juice box. In her severe case, this is her solution to the problem of low sodium. This information is very timely for me personally because all signs point to secondary AI in my near future after radiation and removal of my pituitary gland in my ongoing effort to beat Cushing’s. I feel lucky to have spent a weekend witnessing the adaptive behaviors of people who manage AI in their lives.
Adrenal Insufficiency United is a volunteer-run patient organization focused on helping patients safely and successfully find solutions for their lives with AI. Some patients reach remission from their Cushing’s and are able to avoid AI, but for those who have no choice but to integrate it into their “new normal”, support and advice from others with the same affliction can be just as important as clinical treatment from your doctor. If AI is an issue for you, we highly recommend that you visit AIU’s website at aiunited.org or find them on Facebook.
by Leslie Edwin
Summer, 2018




Sorry, comments are closed for this post.