Introduction
This article reviews the features of cyclical hypercortisolism (overproduction of cortisol). Cyclical hypercortisolism can lead to considerable clinical dilemmas which are discussed below. Cyclical Cushing’s syndrome is a pattern seen in which the overproduction of cortisol fluctuates within a set rhythm. Before discussing this more it is important to realize that in other cases of Cushing’s the production of cortisol is not fixed at the same level from day to day. The production may be episodic with no apparent rhythm. These types of cases can often be associated with fluctuating symptoms and signs.
This particular type of Cushing’s syndrome was once considered to be very rare but is now being increasingly recognized. The phenomenon is important because, if not recognized, it can lead to errors in reaching a diagnosis of the disease and this of course can unfortunately be rather slow. It can also cause difficulties in unravelling the precise cause of the syndrome once a diagnosis has been made. In addition, if the cortisol production is cyclical or episodic then it is much more difficult to assess the success or otherwise of surgery or drugs used as treatment. All of these can, unfortunately, have serious clinical consequences.
Making a Diagnosis of Cyclical Cushing’s Syndrome and its Implications
Clinical researchers, including my own group in Belfast have developed criteria, study protocols and biochemical tools to detect cycling in patients with hypercortisolism. Unfortunately the mechanisms causing the abnormality have not as yet been discovered but some recent insights have been gained. The rest of this article discusses the history of the condition, and then strategies for diagnosing and managing this important subgroup of patients.
Significant cortisol fluctuations in Cushing’s syndrome were first recognized in 1956 by Birke and colleagues(1). They reported large swings in the urinary output of steroids in a lady described as having all the classic symptoms of Cushing’s syndrome. Repeated measurements confirmed large cyclical fluctuations about every 10 days over a study lasting 40 days. In retrospect this is probably the first such case, although that honour is usually ascribed to Bailey who published another case in 1971(2). He presented evidence for cycles of production in a patient with a slow-growing malignant lung tumor (carcinoid type). Subsequent to this there were further sporadic and rare reports of this type of case.
We now define true cyclicity as needing at least three peaks and two troughs of cortisol production (see Fig. 1) to establish the diagnosis. If there is no pattern but a lot of variation then this is described as being intermittent or fluctuating in nature.
In 1985 our group reported the first series of patients with the condition (3). Until that series these cases were thought to be both unusual and rare but we reported 5 well-established cases of cyclical Cushing’s syndrome in a series of 14 patients with hypercortisolism. In 1992 we reported a further three patients whom we studied after transsphenoidal microsurgery for Cushing’s disease because their symptoms and signs were slow to settle and/or because they had variable endocrine results (4). All were established as having cyclical Cushing’s syndrome, first diagnosed postoperatively. We suggested then that this may be a much more common finding than previously recognized and emphasized the need for detailed and ongoing endocrinological investigation after pituitary surgery for hypercortisolism. Our more recent studies have borne this out. In a report of the long-term outcome in 63 patients who had pituitary surgery for the treatment of Cushing’s disease we described our detailed follow-up of the 45 patients who achieved apparent remission immediately after surgery. Of these 45 patients, 10 had late relapses and, of those 10, 6 demonstrated definite cyclical cortisol production (5).
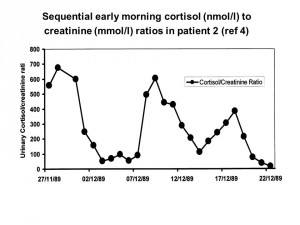
Figure 1: Sequential early morning cortisol (nmol/l) to creatinine (mmol/l) in Patient 2. Used with permission from reference (4).
Establishing the Diagnosis
Cortisol cycling has been defined as occurring when at least three peaks and two troughs of cortisol production are demonstrated by biochemical tests. This often requires prolonged and continuous patient studies and therefore detecting cyclical Cushing’s has been a significant challenge to endocrinologists as 24-hour urinary free cortisol sampling is time-consuming and laborious for any patient. When we first began to study the cyclical phenomenon we performed a study comparing the 24-h urinary cortisol/creatinine ratio with the early-morning ratios and found a close relationship. We were able to confirm that sending small samples of the first morning urine was a scientifically valid way to look at cortisol production from day to day. These experiments have allowed us to follow patients for prolonged periods with the patient posting daily urine samples from home.
Salivary samples could also be used in a similar way in centres that have well established normal ranges. One such case has been reported by Hermus et al (6) in which the patient had cyclical Cushing’s syndrome. Although reports on its use for demonstrating cyclicity are sparse, salivary measurement of cortisol may eventually prove to be a relatively easy way to establish patterns of secretion over extended periods.
Types of Cycle
In general most cases have one type of regular cycle, with cycle lengths varying between 12h and 85 days having been reported. There have been a few patients for whom more complex patterns have been reported. In general, however, the vast majority of cases will emerge as cyclical if a continuous study of 28 days is performed. This is our standard procedure when we suspect the diagnosis and when the clinical condition permits prolonged study.
Clinical Consequences
In every case where possible Cushing’s syndrome is being assessed a serious clinical decision has to be made at some time point as to how far to take investigation, as no one test is infallible. The decision should be based on the clinical index of suspicion plus enough tests for an experienced endocrinologist to be confident that, in all probability, Cushing’s syndrome has been excluded. In some cases this testing may need to include prolonged assessment for cyclicity. It should be made by an endocrinologist experienced in management of Cushing’s syndrome.
In sorting out the exact cause of the Cushing’s it has to be noted that cyclicity has been associated with all of the various causes. It can lead to incorrect interpretation of differential diagnostic tests such as petrosal sinus sampling and the high-dose dexamethasone test with subsequent incorrect management decisions. The investigator has to be aware of this and look carefully at this possibility in all cases.
Can drugs help cyclical Cushing’s?
Cycles of steroid production in normal people have been reported, suggesting that cyclical Cushing’s may simply be an exaggeration of the normal cyclical variation in a subgroup of patients (for further discussion of this see ref 7). Other proposed mechanisms of central cycling of pituitary ACTH and thereby cortisol have included cyclical changes in activation of nervous system control of the pituitary. In our report of five cases of cyclical Cushing’s we used the dopamine agonist bromocriptine and the serotonin antagonist cyproheptadine, either alone or in combination, in four patients with very limited success. The same disappointing results have been obtained by others so presently the usual operative methods of treatment are recommended (3).
Conclusions
Cyclical Cushing’s is a more common type of hypercortisolism than previously thought and it can be rather difficult to diagnose. It should be considered in people with features of hypercortisolism, but documented normal cortisol values, or in patients with fluctuating serum cortisol levels and unusual responses to dexamethasone testing. It should also be considered after pituitary surgery in those patients with low serum cortisol values basally or following dexamethasone testing, but in whom the features of hypercortisolism are slow to resolve or in whom there is evidence of clinical relapse. Fluctuation is a problem in assessing therapy in Cushing’s patients. Normal cortisol levels on one or a few occasions after surgery do not allow cure to be assumed. This applies equally well to studies using drugs instead of surgery. Our higher than average index of suspicion for this form of hypercortisolism, and our ability to diagnose it easily using consecutive early-morning urine tests has enabled us to diagnose relapse at an earlier and more subtle stage and to assess response to drugs better. Further studies of the effect of drugs such as sodium valproate and other centrally active drugs would be warranted, including the newer somatostatin analogues.
Endocrinologists should be aware of the possibility of cyclical oversecretion of cortisol in all patients with discordant clinical and biochemical findings. Collection of tests initially over 28 days confirms or rules out the diagnosis in the vast majority of cases. Salivary cortisol estimations have great potential for diagnosis but this remains to be confirmed. The mechanisms for cycling production remain unclear but I suspect that abnormal responses to other rhythmical local factors may be responsible.
Author: A. Brew Atkinson MD DSc FRCP FRCPI (Spring, 2009)
Editor’s Note: Professor Brew Atkinson is currently head of the Regional Centre for Endocrinology and Diabetes at the Royal Victoria Hospital and Professor of Endocrinology, Queen’s University, both in Belfast, Northern Ireland, UK. He has worked there since 1981 after qualifying in medicine from Queen’s and then completing postgraduate training in Belfast, Glasgow (Scotland) and in Vanderbilt University (Nashville USA). He has had a longstanding interest in the diagnosis and management of Cushing’s syndrome.
References
- Birke,G, Diczfalusky,E,Plantin,L (1956) Fluctuation in the excretion of adrenocortical steroids in a case of Cushing’s syndrome J Clin Endocrinol 16:286-290
- Bailey, RE (1971) Periodic hormonogenesis – a new phenomenon. Periodicity in function of a hormone producing tumour in man J Clin Endocrinol 32:317-320
- Atkinson, AB, Kennedy, AL, Carson, DJ, et al (1985) Five cases of cyclical Cushing’s syndrome Br Med J (Clin Res Ed) 291:1453-1457
- Atkinson, A.B, McCance, DR, Kennedy, L, Sheridan, B (1992) Cyclical Cushing’s syndrome first diagnosed after pituitary surgery: a trap for the unwary Clin Endocrinol (Oxf) 36:297-299
- Atkinson, AB, Kennedy, A, Wiggam, MI et al (2005) Long-term remission rates after pituitary surgery for Cushing’s disease: the need for long-term surveillance Clin Endocrinol (Oxf) 63:549-559
- Hermus,AR, Pieters,GF, Borm,GF et al (1993) Unpredictable hypersecretion of cortisol in Cushing’s disease: detection by daily salivary cortisol measurements Acta Endocrinol (Copenh) 128:428-432
- Glass, AR, Zavadil, AP, Halberg, F et al (1984) Circadian rhythm of serum cortisol in Cushing’s disease J Clin Endocrinol Metab 59:161-165




Sorry, comments are closed for this post.