Introduction
Memory issues in Cushing’s patients have been reported in the literature over the years however, the number of studies addressing this issue is limited. With the fairly recent advent of new imaging techniques, investigators can now study both the physical structure of the brain and brain metabolites (biochemical compounds) in greater detail using non-invasive techniques. These imaging techniques, when combined with memory tests, can give investigators greater insight into the memory impairment observed with increased levels of cortisol (hypercortisolism).
What do we know about hypercortisolism and memory impairment?
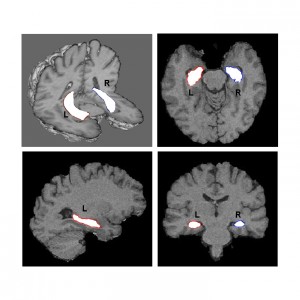
Figure 1 – The hippocampus is shown in white in different views of a single individual on these MRI’s.
How is memory evaluated in Cushing’s patients and the normal population?
There are 2 different tests, one for verbal memory and one for visual memory. To test verbal memory, in the Rey Auditory Verbal Learning Test (RAVLT), patients and normal controls are asked to memorize a list of words and to repeat it. Verbal memory has been related to left hippocampal volume. For visual memory (ROCF memory test), patients and normal controls are asked to draw a diagram with and without the diagram in front of them and after varying periods of time. Visual memory has been related to the right hippocampal volume. Both of these tests have been validated for normal ranges of function in very large populations.
What is known about the relationship of hippocampal volume and memory in Cushing’s patients?
In a recent study, we evaluated performance on memory tests and measured hippocampal volume using 3 tesla MRI in 33 Cushing’s patients, (11 with active disease and 22 cured) and in normal age matched controls (Resmini et al 2012). This study found that both verbal and visual memory performance were worse in Cushing’s patients compared to controls, however, only the 12 patients with severe memory impairments (below normal values) showed reduced hippocampal volumes. Generally these patients tended to have a longer duration of active Cushing’s, have less education, and were roughly 8 years older. Thus hippocampal volume does not seem to account for all the memory issues associated with Cushing’s.
What about other parts of the brain?
In the same study, the total brain grey matter volumes, both cortical and subcortical, of Cushing’s patients and controls were evaluated. A reduction in total and cortical gray matter volumes was found in Cushing’s patients compared to normal controls. Age is known to decrease brain volume, however, slightly over 50% of Cushing’s patients showed lower cortical brain volumes than expected for their age, compared to 6% of controls. Subcortical atrophy was observed only in those patients with severe memory impairment.
Are there other things in the brain that can be studied?
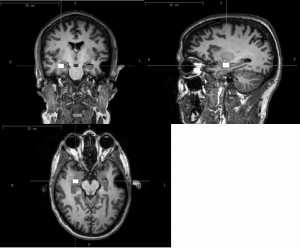
Figure 2 – The volume of interest (VOI) is shown in white in different views of the same individual. This was the area of the hippocampus where brain metabolites were measured.
The brain is composed of cells called neurons (grey matter) that communicate with each other and control the thinking and memory processes. White matter of the brain is composed of glial cells which support the neurons by delivering nutrients and cleaning up debris should a neuron die. Glial cells and neurons have different biochemical compositions. By assessing concentrations of biochemical components, 1H-MRS can indirectly deliver information on glial and neuronal integrity, potential cell loss and biochemical alterations in the brain. For this reason, we used 1H-MRS to study hippocampal metabolites in Cushing’s patients.
Do cured Cushing’s patients have normal levels of brain metabolites?
Using 1H-MRS, we demonstrated, for the first time, that abnormal levels of certain brain metabolites in the head of both the right and left hippocampus of Cushing’s patients persist despite endocrine cure of hypercortisolism (Resmini et al 2013). Low levels of the metabolite NAA were observed compared to healthy controls. This indicates neuronal dysfunction and/or loss. High levels of the metabolite Glx were also observed, suggesting that the number of glial cells increased as a repair mechanism to increase brain volume. These altered brain metabolite profiles could be considered early markers of glucocorticoid neurotoxicity and would precede hippocampal volume reduction and could be involved in the memory impairments evidenced in these patients. These alterations would explain the lower memory performance in Cushing’s patients with normal hippocampal volumes. Thus, an earlier diagnosis and a rapid normalization of hypercortisolism could avoid the progression of hippocampal damage and memory impairments.
Why is this important to patients and clinicians?
Patients need to keep in mind that while individual patients generally report memory improvements following cure and most return to memory function in the normal range, the patient may notice that their memory is not quite at the level of previous performance, even though it is in the normal range. Other patients may experience persistent severe memory impairments. If patients perform regular memory exercises, they may also maintain or even improve their memory.
Less exposure to hypercortisolism by earlier diagnosis and successful treatment of Cushing’s would probably avoid the progression of memory problems and the reduction of hippocampal volume. This is an important take home message for clinicians for the daily management of these patients. Further longitudinal studies of patients before and after normalization of cortisol would be needed to clarify all the points opened by these preliminary observations. Future research in the field should evaluate if these chemical abnormalities are present in the whole brain of Cushing’s patients and if patients using high levels of glucocorticoid drugs have the same brain alterations, causing memory problems. This represents a new challenge in the endocrine field, connecting neuroendocrinology to daily life in clinical practice.
References:
Eugenia Resmini, Alicia Santos, Beatriz Gómez-Anson, Yolanda Vives, Patricia Pires, Iris Crespo, Maria J Portella, Manel de Juan-Delago, Maria-José Barahona, and Susan M Webb
Verbal and visual memory performance, hippocampal volumes by means of 3 tesla magnetic resonance imaging, in patients with Cushing´s syndrome
J Clin Endocrinol Metab. 2012 Feb;97(2):663-71.
Eugenia Resmini, Alicia Santos, Beatriz Gómez-Anson, Olga López-Mourelo, Patricia Pires, Yolanda Vives-Gilabert, Iris Crespo, Maria J. Portella, Manel de Juan-Delago, and Susan M Webb
Hippocampal dysfunction in cured Cushing’s syndrome patients, detected by 1H-MR-spectroscopy
Clin Endocrinol (Oxf). 2013 Nov;79(5):700-7.
Author: Eugenia Resmini, MD, PhD (Spring, 2014)
Editor’s Note: Dr. Resmini is with the Centro de InvestigaciónBiomédica en Red de EnfermedadesRaras (CIBER-ER, Unidad 747), Instituto de InvestigaciónBiomédica (IIB)-Sant Pau, ISCIII, Hospital Sant Pau, Endocrinology/Medicine Department and UniversitatAutònoma de Barcelona, Spain, where she is a postdoctoral medical assistant. She has extensive experience in pituitary disorders.




Sorry, comments are closed for this post.