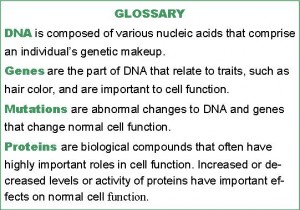
Cushing’s patients often ask their physicians what caused their rare disease; they want to know if it has anything to do with their DNA and whether it can be inherited. Changes in the building blocks of genes (i.e., mutations) do indeed play a role in the development of tumors that increase adrenocorticotropic hormone (ACTH) or cortisol secretion. It is important to understand that different types of mutations occur:
- Inheritable mutations (germline mutations) are present in an individual’s DNA from conception. These are inherited from the parents and can be passed on to their children.
- Non-inheritable mutations (i.e., sporadic mutations) occur after birth, most often in a single cell. These mutations are not inherited from the parents and cannot be passed on to their children.
 Most ACTH-secreting pituitary tumors (Cushing’s disease) are not hereditary and result from a mutation to a single ACTH-secreting cell sometime after birth. There is a syndrome called multiple endocrine neoplasia type 1 that can be hereditary, but Cushing’s disease is extremely rare in this condition.
Most ACTH-secreting pituitary tumors (Cushing’s disease) are not hereditary and result from a mutation to a single ACTH-secreting cell sometime after birth. There is a syndrome called multiple endocrine neoplasia type 1 that can be hereditary, but Cushing’s disease is extremely rare in this condition.
A single cortisol-secreting tumor on one adrenal gland is also not hereditary; thus the mutation involved occurs after birth. Some cases of bilateral adrenal hyperplasia, which means both adrenal glands are enlarged, have been shown to be hereditary.
Normally, the body tightly controls cortisol production by a feedback system. The pituitary gland secretes ACTH, which then circulates in the bloodstream and acts on the adrenal glands to stimulate cortisol production. Increased cortisol levels send a signal to the pituitary gland to decrease ACTH secretion, in order to maintain cortisol at normal levels.
Cells have complex, built-in mechanisms to control growth and regulate cell function. When these mechanisms become abnormal, tumors or enlargement of tissues may occur, and increased function, such as elevated ACTH secretion and cortisol production, which are less subject to the feedback mechanisms, results. Researchers have investigated the genetic changes that might be involved in the formation and function of pituitary tumors, adrenal tumors, and adrenal enlargement (hyperplasia). Within the last year, several publications have studied the possible mechanisms by which this happens.
Cushing’s Disease
The cause of Cushing’s disease (an ACTH-secreting pituitary tumor) is overgrowth of one ACTH-producing cell in the pituitary, which multiplies abnormally to become a benign tumor that produces too much ACTH; this causes a continuous signal to the adrenal glands to secrete cortisol. The genes responsible for the abnormal growth of a pituitary ACTH-secreting cell have not been identified. New genetic methods have been used to find mutations in genes that are particularly important in ACTH-producing cells, but studies have not yet identified one gene that is common to most pituitary tumors. However, in recent months, abnormal levels of certain proteins were found in the pituitary tumors removed from patients with Cushing’s disease.
One protein, called testicular orphan receptor 4 (TR4), was found in higher quantities than normal in human Cushing’s disease tumors and was shown to stimulate ACTH secretion and tumor growth in cells in test tubes. Additional studies are needed to determine if this receptor can explain the development of pituitary tumors and if drugs could be targeted to decrease its levels [1].
Another protein found in high quantities in such tumors is called pituitary transforming gene (PTTG). This protein regulates important signals that stimulate cell multiplication. A drug called R-roscovitin, which targets this regulator, was able to decrease ACTH, cortisol production, and tumor growth in animal models [2]. This information is still very preliminary, but it introduces new targets for further study and suggests new drugs that could be used in the future to treat patients with Cushing’s disease.
Adrenal Tumors
In most cases, adrenal Cushing’s is caused by a single benign adrenal tumor (adenoma) on one adrenal gland. While adrenal Cushing’s is relatively rare, adrenal tumors are not uncommon as they are found in approximately 4% of individuals over 50 years of age. Not all adrenal tumors, however, produce excess hormones. While obvious Cushing’s is observed in some patients with an adrenal tumor, a mild degree of cortisol excess with few obvious symptoms, termed subclinical Cushing’s, is observed in many patients and could contribute to several conditions such as the metabolic syndrome, hypertension, and osteoporosis in these patients.
Several different mutations have been identified in adrenal adenomas; however, they seemed to be important in only a very few cases. A recent multinational study led by German researchers [3] investigated a number of adrenal adenomas for mutations. This study included 139 adrenal adenomas, 59 of which caused obvious Cushing’s syndrome, 40 of which caused subclinical Cushing’s syndrome, 20 of which produced aldosterone, and 20 of which were nonfunctional. These researchers found mutations of the PRKACA gene that increased the activity of protein kinase A, which is known to be important in the secretion of cortisol. This mutation was found in 37% of adrenal adenomas from patients with obvious Cushing’s syndrome. This particular mutation was not found in normal adrenal tissue, nonfunctioning adrenal adenomas, tumors producing aldosterone, or those producing subclinical Cushing’s syndrome. This indicates that subclinical Cushing’s could be a distinct disorder that may not progress to obvious Cushing’s. This specific mutation was not found in cells outside of the tumor, indicating that this mutation occurred after birth.
This finding was confirmed by Chinese researchers [4] who also found sporadic mutations in the same PRKACA gene in 65.5% (57/87) of cortisol secreting adrenal adenomas and was also shown to increase protein kinase A activity.
Bilateral Adrenal Hyperplasia
Bilateral adrenal hyperplasia is the cause of less than 2% of adrenal-based Cushing’s syndrome. However, about 10% of adrenal abnormalities found by accident on an abdominal computed tomography scan are bilateral. Some of these lead to subclinical Cushing’s, which is more common than obvious Cushing’s. Some cases of bilateral adrenal hyperplasia have been reported to occur in families, indicating that inherited genetic defects are involved.
Primary Pigmented Nodular Adrenocortical Disease (PPNAD)
PPNAD is an adrenal disorder where very small nodules are found in both adrenals; it can run in families and be associated with the Carney Complex. Patients with Carney complex can also develop tumors in the heart and other endocrine tissues and have increased skin pigmentation. PPNAD and Carney complex have been extensively studied and inheritable mutations of important genes PRKAR1A, PDE11A or PDE8B, which regulate signals to produce cortisol, have been identified in a large number of affected patients. [5].
Bilateral Macronodular Adrenal Hyperplasia
As with adrenal adenomas, some mutations have been reported in bilateral macronodular adrenal hyperplasia tissue (i.e., enlarged adrenals with multiple large nodules); however, there is not one individual mutation that was shared among a large number of patients. With bilateral macronodular adrenal hyperplasia, as cortisol becomes elevated, ACTH is suppressed, so the hyperplasias were termed ACTH-independent. Research over the past 20 years [6] has shown that some patients with bilateral macronodular adrenal hyperplasia show increased cortisol production in response to hormones other than ACTH , such as gastric inhibitory polypeptide (GIP), vasopressin, adrenalin, serotonin, and human chorionic gonadoptropin (hCG), but the genetic basis of the hyperplasia remained a mystery.
A recent series of studies [7, 8,] looked at bilateral macronodular adrenal hyperplasia tissue and found a mutation in a gene called ARMC5. This mutation was found in 25%–55% of two groups of French and American patients with apparently non-inherited, sporadic Cushing’s syndrome. On further investigation, it was found that the adrenal nodule contained an inheritable germline mutation as well as a sporadic mutation. The hyperplasia cells that were not in the nodules contained only the inheritable germline mutation. Approximately 50% of first-degree relatives carried the inheritable germline mutation and had unsuspected subclinical Cushing’s and bilateral macronodular adrenal hyperplasia. While the function of ARMC5 is not known, it was shown to be present in lower quantities in the adrenal tissues of patients with the mutation. It was also shown that inactivation of ARMC5 led to greater cell growth, perhaps leading to hyperplasia and also to changes in cortisol production. Another study found similar ARMC5 mutations in families with bilateral macronodular adrenal hyperplasia from Brazil [9]. Carriers of the mutation were found to develop adrenal nodules as young adults but some initially presented with only one enlarged adrenal gland.
These studies point out the importance of examining family members of patients with bilateral macronodular adrenal hyperplasia to detect possible silent carriers of the same disease and those with subclinical Cushing’s syndrome.
Another study [10] also looked at bilateral macronodular adrenal hyperplasia tissue from 30 patients and very surprisingly found that ACTH was produced in adrenal cells in all 30 patients. This was not observed in normal adrenal tissue or adrenal adenomas. In addition, stimulation of cells with GIP, serotonin, and hCG caused an increase in ACTH secretion in tissue from patients who showed abnormal responses to these hormones. Compounds that decreased the ability of ACTH to stimulate cortisol secretion greatly reduced cortisol secretion from these tissues. Thus, these newer compounds currently under development might be useful for treatment of select patients. It now appears that bilateral macronodular adrenal hyperplasia should no longer be classified as being ACTH-independent.
Chinese researchers also reported somatic non-inheritable mutations in proteins called histones in isolated cases of bilateral macronodular adrenal hyperplasia [4]. This preliminary report will need to be confirmed.
Summary
In summary, the genetic basis for pituitary tumors responsible for Cushing’s disease is still unknown, but new target proteins that can regulate their growth are under study. The cause of adrenal adenomas causing Cushing’s syndrome has now been identified in a large percentage of cases. Inherited mutations have been identified in patients with PPNAD and bilateral macronodular adrenal hyperplasia, and it is likely that there will be advances in genetic screening tools to detect affected family members at a much earlier stage than before. While the work discussed is promising and the ultimate goal is to have highly effective pharmaceuticals based on what we now know, translating genetic findings into treatment options is a long-term project.
Authors: Dr. André Lacroix and Karen Campbell (Spring, 2014)
Editor’s Note: Dr. André Lacroix is Professor, Department of Medicine at University of Montreal teaching hospital (CHUM) where he treats Cushing’s patients and does research in the area. Karen Campbell hold a MS degree in Molecular Biology and is a Director of CSRF.
References
- Du L, Bergsneider M, Mirsadraei L, Young SH, Jonker JW, Downes M et al. Evidence for orphan nuclear receptor TR4 in the etiology of Cushing disease. Proc Natl Acad Sci U S A 2013; 110(21):8555-8560.
- Liu NA, Jiang H, Ben Shlomo A, Wawrowsky K, Fan XM, Lin S et al. Targeting zebrafish and murine pituitary corticotroph tumors with a cyclin-dependent kinase (CDK) inhibitor. Proc Natl Acad Sci U S A 2011; 108(20):8414-8419
- Beuschlein, F, Fassnacht M, Assié G, Calebiro D, Stratakis, C, et al. Constitutive activation of PRKACA in adrenal Cushing’s syndrome. N Engl J Med 2014; 370:1019-1028
- Cao Y, He M, Gao Z et al. Activating Hotspot L205R Mutation in PRKACA and Adrenal Cushing’s Syndrome. Sciencexpress, April 3 2014, [DOI:10.1126/science.1249480]
- Statakis, CA, New genes and/or molecular pathways associated with adrenal hyperplasias and related adrenocortical tumors. Mol Cell Endocrinol. 2009 Mar 5;300(1-2):152-7. doi: 10.1016/j.mce.2008.11.010. Epub 2008 Nov 21.
- Lacroix A, Bourdeau I, Lampron A, Mazzuco TL, Tremblay J, Hamet P. Aberrant G-protein coupled receptor expression in relation to adrenocortical overfunction. Clin Endocrinol (Oxf) 2010; 73(1):1-15
- Assie G, Libe R, Espiard S, et al. ARMC5 mutations macronodular adrenal hyperplasia with Cushing’s syndrome. N Engl J Med 2013; 369:2105-2114
- Faucz FR, Zilbermint M, Lodish MB, Szarek E, Trivellin G, Sinaii N et al. Macronodular Adrenal Hyperplasia due to Mutations in an Armadillo Repeat Containing 5 (ARMC5) Gene: A Clinical and Genetic Investigation. J Clin Endocrinol Metab March 6 2014 jc20134280
- Alencar GA, Lerario AM, Nishi MY, Mariani BMM, Almeida MQ, Tremblay J, Hamet P, Bourdeau I, Zerbini MCN, Pereira MAA, Gomes GC, Rocha MDS, Chambo JL, Lacroix A, Mendonca BB, Fragoso MCBV. ARMC5 Mutations are a Frequent Cause of Primary Macronodular Adrenal Hyperplasia.. J Clin Endo Metabol ; April 7 2014, jc20134237. [Epub ahead of print]
- Louiset E, Duparc C, Young J, et al. Intraadrenal production of corticotropin in maronodular bilateral adrenal hyperplasia causing Cushing’s syndrome. N Engl J Med 2013; 369:2115-2125




Sorry, comments are closed for this post.