Post-operative recovery from Cushing’s syndrome (CS) can be difficult for patients. Although the impaired health-related quality of life in active CS improves after surgical remission, the quality of life does not normalize in all. Despite extensive research on post-surgical recovery from CS, little research has examined the patient experience recovering from remission of CS. In an open-ended survey distributed through the Cushing’s Support and Research Foundation (CSRF), 84% of 94 patients described their recovery process as negative. To build upon these findings, we aimed to characterize better the patient experience of recovery and compare this experience to the perspective of endocrinologists.
To do this, we developed 2 web-based surveys: one for patients successfully surgically-treated for CS, promoted through the CSRF, and the other for endocrinologists, promoted through adult endocrinology programs in the United States and United Kingdom, and the Pituitary Society. No personally-identifiable information was collected. Both surveys asked questions related to the overall recovery experience, difficulties faced by patients, helpful resources during recovery, support offered by doctors, and cortisol replacement medication (CRM). 389 patients and 60 physicians completed the surveys. Patients completed the survey a median of 36 months after their last surgery. The physicians who completed the survey saw a median of 10 patients each year with surgically-treated CS.
We found that patient-defined recovery takes longer than physicians realize. Although there was overlap, there was a significant difference between the time physicians believed patients completely recovered and the time patients reported full recovery: a median of 12 months vs. 16 months (p=0.03, Figure 1). There was also a significant difference between the perceived time to discontinue CRM after surgical treatment of CS: physicians reported a median of 9 months while patients reported 8 months (p=0.04).
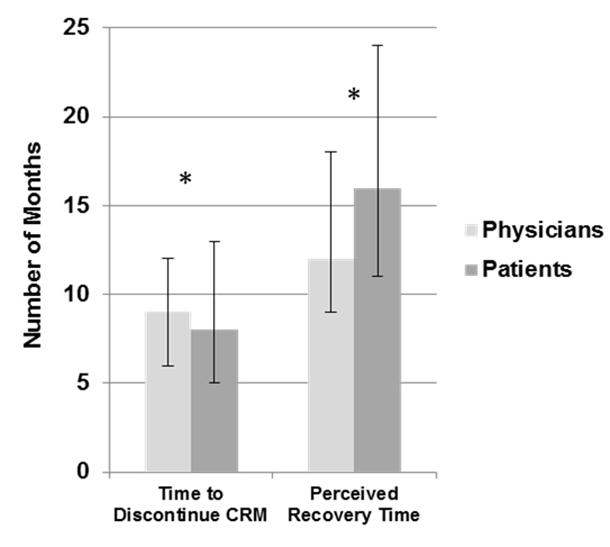
Figure 1: Median time reported by patients to discontinue cortisol replacement medication (CRM) and fully recover following successful surgical treatment for Cushing’s syndrome, compared with the median time reported by physicians; error bars indicate interquartile range, *p < 0.05
There were discrepancies between the resources patients reported receiving from their doctors about the post-surgery recovery experience and those that doctors reported providing to their patients. 40% of patients (n=87/217) reported not receiving any information about the post-surgery recovery experience from a health professional. 29% reported receiving information from only their endocrinologists, 17% from only their neurosurgeon, and 25% from both their endocrinologists and neurosurgeon. However, 100% of physicians (n=49/49) reported discussing with patients verbally the recovery experience after their surgical treatment and 39% reported providing their patients with written information about the recovery process. These results suggest that multiple education modalities that include both written material and verbal discussions may be useful to patients. Also, as shown in Table 1 below, patients and physicians differed in what they deemed most helpful during the recovery process.
| Patients | Physicians |
| 1. Family and Friends | 1. Family and friends |
| 2. Rest | 2. Exercise |
| 3. Education | 3. Activities |
| 4. Exercise | 4. Work |
| 5. Activities | 5. Support Groups |
| Table 1: Top 5 most helpful resources during recovery reported by patients and physicians |
|
Although these results provide further insight into the daunting challenge faced by patients recovering from CS after surgical treatment, further research is needed to identify factors that contribute to the degree of long-term impairment described during recovery from CS. 59% of physicians (n=16/27) described patient’s overall recovery experience following successful surgery as mixed, 22% as negative, and 19% as positive. Patients reported similar rates (p=0.84): 61% of patients (n=161/264) described their overall recovery experience after successful surgery as mixed, 15% as negative, and 24% as positive. By learning more about the recovery process, we hope to identify specific ways to improve the patient experience during recovery in the future.
Authors: Brent Abel1, Nicola M. Neary1, Karen Campbell2, and Lynnette K. Nieman1
1National Institutes of Health, Bethesda, Maryland
2Cushing’s Support and Research Foundation (Summer, 2012)




Sorry, comments are closed for this post.