Pituitary adenomas represent 10 to 20% of all intracranial lesions. One of the most challenging pituitary adenomas from a treatment standpoint is ACTH-secreting adenomas. These tumors can be difficult to discern on MR imaging, and, even in the hands of an experienced neurosurgical team, some patients may not achieve remission after transsphenoidal or transcranial resection of the adenoma.
Historically, external beam radiation therapy was the adjuvant treatment of choice for recurrent or residual pituitary adenomas. More contemporary data has demonstrated serious limitations of conventional radiotherapy in treating Cushing’s disease– the time to hormonal normalization is slow and the rate of post-procedural hypopituitarism is high. Although Cushing’s disease is a serious health problem if left untreated, many physicians became concerned that with radiation therapy that the “cure” was worse than the disease.
Stereotactic radiosurgery was investigated as a treatment option for persistent Cushing’s disease. The advantages of stereotactic radiosurgery over conventional radiation therapy include a higher biologic equivalent dose, steep fall off, image guidance, and small treatment volume. Moreover, the serious risks of hypopituitarism, stroke, and other radiation induced injury appear to be substantially less with radiosurgery.
Shortly after radiosurgery’s development, Lars Leksell treated patients with pituitary tumors using the Gamma Knife; original localization was achieved through use of plain radiographs of the sella. With more recent advances in neuro-imaging including Positron Emission Tomography (PET) scans and fat saturation MRI, the Gamma Knife and other radiosurgical devices have been utilized to control adenoma growth and normalize hormone over-production for many Cushing’s patients.
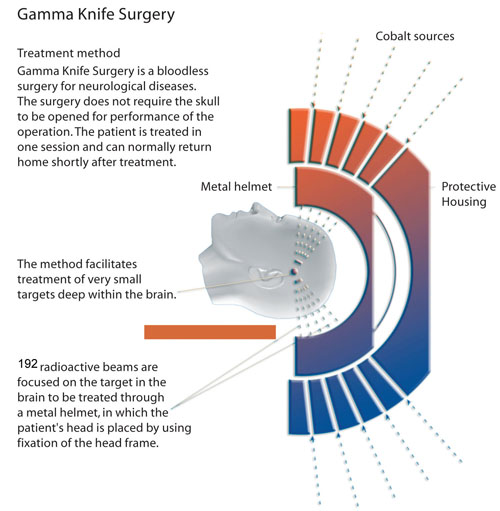
Gamma Knife radiosurgery (GKRS) represents a minimally invasive neurosurgical option for the treatment of Cushing’s disease, and it is usually reserved as a second line treatment following an initial, unsuccessful attempt at a microsurgical cure. GKRS involves multiple isocenters of different beam diameter to achieve a dose plan that conforms to the irregular three-dimensional volumes of most mass lesions. The total number of isocenters varies depending upon the size and shape of the adenoma and the proximity of surrounding at risk structures (e.g. the optic nerves or chiasm). The most recent version of the Gamma Knife, the Perfexion, combines advances in dose planning, collimation of 192 simultaneous beams, and robotic engineering, and it eliminates the need to set coordinates manually for each isocenter.
The goals of stereotactic radiosurgery in the treatment of Cushing’s disease pituitary tumors are to inactivate adenoma cells, controlling tumor growth and to normalize hormone overproduction. Ideally, these goals are met without damaging the residual normal pituitary gland and surrounding vascular and neuronal structures.
Most centers define an endocrine remission for Cushing’s disease as a 24 hour urine free cortisol in the normal range associated with the resolution of clinical stigmata or a series of normal post-radiosurgical serum cortisol levels obtained throughout the day. In our institutional experience of treating 107 patients with Cushing’s disease, the remission rate was 53% and the vast majority achieved adenoma volume control (i.e. shrinkage or no growth of the pituitary adenoma). In general, most patients who ultimately demonstrated hormonal normalization did so within the first 2 years following radiosurgery. Recent work suggests that ketaconazole and other cortisol suppressive medications may adversely affect the endocrine outcome following GKRS. As such, a temporary cessation of such cortisol lowering agents at the time of radiosurgery seems prudent.
Potential complications following Gamma Knife radiosurgery for Cushing’s disease include delayed hypopituitarism which occurs in approximately 20-30% of cases and an extremely rare chance of visual dysfunction. Careful longitudinal follow up of Cushing’s patients including serial MRI’s, neurological, and endocrine evaluations are important.
Although surgical resection still represents the initial treatment option for most patients with Cushing’s disease, Gamma Knife radiosurgery represents a safe and predominantly effective treatment option for patients with recurrent or persistent Cushing’s disease following an initial resection. The benefits and risks of Gamma Knife radiosurgery are best decided in the context of a comprehensive and multidisciplinary review of a particular patient’s case. Just as is true for other treatment options for Cushing’s disease, long-term follow up is also required after GKRS.
Author: Jason Sheehan, MD, PhD (Winter, 2008)
Editor’s Note: Dr. Sheehan completed his residency in neurosurgery at the University of Virginia and a fellowship at the University of Pittsburgh. Currently, he is an Assistant Professor of Neurological Surgery and Radiation Oncology at the University of Virginia and is the Director of the University of Virginia’s Gamma Knife Center.




Sorry, comments are closed for this post.