Adapted from a presentation at the AIU conference by Dr. Mitchell Geffner, Children’s Hospital of Los Angeles, CA
The structure of cortisol was discovered in the 1930s. By the next decade scientists had developed a way to create a synthetic replacement, a substance known as cortisone. The 1950 Nobel Prize in Physiology or Medicine went to Drs. Edward Kendall, Tadeus Reichstein, and Philip Hench for “their discoveries relating to the hormones of the adrenal cortex, their structure and biological effects” (www.nobelprize.org/nobel_prizes/medicine/laureates/1950). By 1955, hydrocortisone as we know it today was presented to the world.
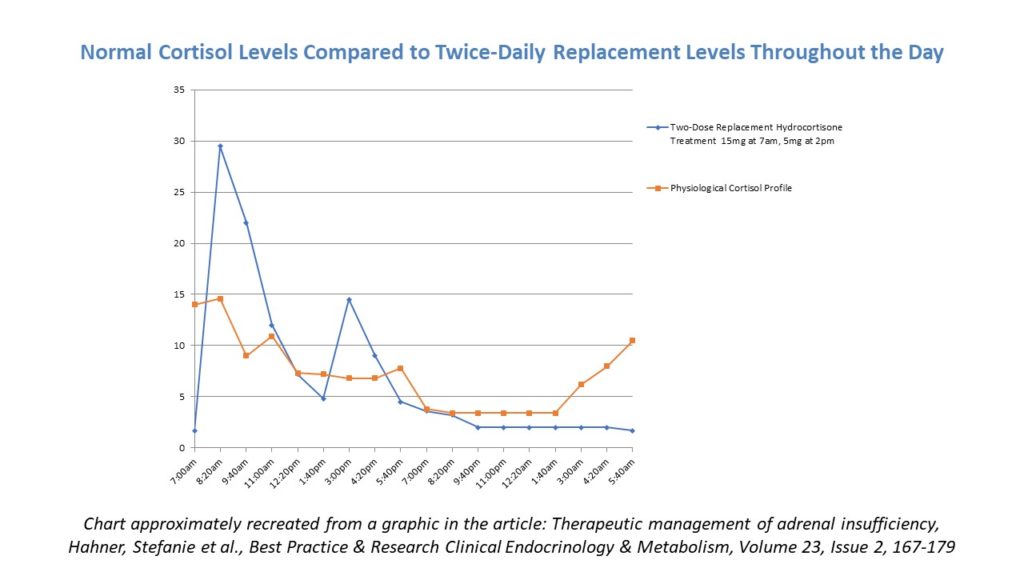
Traditional treatment in temporary and permanent adrenal insufficiency (AI), regardless of the source, tends to be twice-daily hydrocortisone (with the addition of fludrocortisone if the patient has primary AI). Doctors have historically preferred hydrocortisone over others like prednisone and dexamethasone because it is the most physiologically similar to natural cortisol, it is not as strong as the other choices, and it clears the body quickly. The following graphic shows why the two-dose regimen tends to work for the majority of patients who need replacement – it does a satisfactory job of mimicking the natural profile of cortisol in the body.
That being said, Dr. Geffner expressed approval of three doses spread every eight hours to avoid a period of time overnight where a patient would not have any cortisol coverage. Many patients in the audience shared how they split their total daily quantity of hydrocortisone into three or four doses based on experience, activity levels, and to avoid lows or “crashes” in the evening.
There are three hydrocortisone products in development out of the UK that address some of the issues patients can have when hydrocortisone, prednisone, and dexamethasone still leave something to be desired.
Plenadren (manufactured by Shire) is a modified dual-release hydrocortisone with immediate and sustained absorption through its immediate-release coating and extended-release core. In adults, the single morning dose gives similar cortisol exposure to a thrice-daily regime of immediate-release hydrocortisone, although Plenadren tends to provide higher concentrations of cortisol in the late morning and lower concentrations in the late evening than a conventional hydrocortisone schedule. The expectation is that a once-daily dose will improve adherence and quality of life, although this remains to be demonstrated in trials.
Chronocort (manufactured by Diurnal) is a modified-release hydrocortisone that differs from Plenadren in that it has a “delayed and sustained” rather than an “immediate and sustained” absorption profile. Chronocort aims to replace physiological cortisol concentrations by dosing at morning and night. The nighttime dose provides release of hydrocortisone in the early hours of the morning providing a prewaking rise in cortisol levels. A study of Chronocort in 16 adults with Congenital Adrenal Hyperplasia showed that a twice-daily regimen of Chronocort provided a similar cortisol rhythm and early morning peak to physiological cortisol concentrations in healthy volunteers. Whether these short-term effects can be sustained and what effect on overall health status this has in patients is the subject of an ongoing Phase 3 study in the UK. (Porter J, Blair J, Ross RJ, Is physiological glucocorticoid replacement important in children? Archives of Disease in Childhood 2017; 102: 199-205)
Lastly, there is the Hydrocortisone Pump. This technology was pioneered by Professor Peter Hindmarsh of Great Ormond Street Hospital in the UK and is similar to an insulin pump. The scientific community is currently looking at this treatment through trials, but it’s not expected that this will become a common treatment anytime soon. Several patients who use the pump have written blog posts and other first-hand accounts of why they sought it out, the difficulties of getting it, and pros and cons of using a pump vs. more traditional therapy. AI patients who would benefit most from a cortisol pump are:
- those who have rapid metabolism of cortisol in whom adequate control cannot be achieved with conventional replacement, even at 4-5x daily dosing
- those with severe stomach irritation from glucocorticoids
- those for whom life-threatening conditions are a reality because they don’t take their meds on a regular basis, as scheduled
Ultimately, the pump was designed and intended for those who experience extremely diminished quality of life because of their inability to achieve an acceptable level of success with oral cortisol replacement. The pump ensures 100% absorption because the medicine goes straight from the fat into the vein. Users can still stress dose with oral meds for illness.
Summer, 2018




Sorry, comments are closed for this post.