Any endocrinologist familiar with Cushing’s hears from patients that the weight gain associated with Cushing’s is unstoppable, even with calorie restriction and exercise. Several factors have been shown to be causal, including cortisol’s direct effects on fat mass, function, and distribution. Specifically, exposure to excess cortisol increases total fat, and abdominal fat in particular, while reducing muscle mass, thus body composition and fat distribution are altered. (1,2) Cortisol also regulates the process of fat cell development and break down (lipolysis), with an overall effect to increase fat mass and cause insulin resistance and risk for diabetes. (3-7) Finally, cortisol has effects on other hormones, including thyroid, growth hormone, and reproductive hormones, all of which play a role in body composition and weight.
Other factors can indirectly impact weight and fat mass. For instance, cortisol regulates mood and concentration. It has been well demonstrated in the medical literature that depression or anxiety can lead to increased food intake in the normal population. Since these conditions can be present in patients with Cushing’s, depression and anxiety may contribute to increased food intake and thus result in overall weight gain. Cushing’s and/or depression may also reduce energy and activity levels, which could also contribute to weight gain.
I hear from many Cushing’s patients that they are often hungry or crave certain foods. Since cortisol is a flight or fight hormone geared towards ensuring survival, it makes sense that with increased cortisol the brain perceives stress, and thus could initiate eating to ensure that energy stores are available to combat or escape the stressor. These attempts to maintain homeostasis and survival could occur via modulation of appetite, food cravings, and the reward value of food.
It is commonly believed that steroid hormones (e.g. cortisol or other glucocorticoids including prednisone or dexamethasone) “make people hungry.” However, the exact role that cortisol may have in regulating hunger, satiety, and food craving has not been well-studied in humans, and particularly not in patients with Cushing’s. Thus, we undertook the following studies to try to understand some of the mechanisms of cortisol-induced weight gain. Since many patients continue to struggle with weight even after successful treatment of Cushing’s, we were also interested in studying patients with ‘cured’ disease, to try to understand potential lasting effects the prior excess cortisol exposure has on weight.
A prospective study of appetite and food craving in patients with Cushing’s (8)
We first quantified appetite and food craving in 30 people with Cushing’s who were studied prospectively before treatment (with active disease), and again after they had achieved remission, in order to understand the role of excess cortisol exposure in regulating hunger signals and food craving. Since some studies have suggested that body composition and cardiovascular risk factors can persist in Cushing’s patients despite remission, we also looked at predictors of food intake in people with treated Cushing’s.
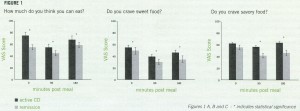
Each patient underwent two detailed study visits at our clinical research unit, one before surgery and one about a year and a half after surgery. Patients arrived fasting in the morning and completed a previously validated visual analogue scale (VAS) questionnaire before and again one and a half and three hours after drinking a test meal which contained 50% carbohydrate, 35% protein, and 15% fat. The VAS questionnaire consisted of lines with words anchored at each end describing extreme sensations of hunger, prospective consumption (“How much do you think you can eat?”), fullness, and satisfaction, as well as craving (sweet, salty, fatty or savory). Patients were asked to mark on the line corresponding to their feelings. Results were calculated by measuring the distance from the left end of the line to the mark.
Blood was also drawn to measure insulin, glucose, and the appetite hormones ghrelin and PYY before and over time after the test meal. Ghrelin and PYY are hormones secreted in the gut that regulate hunger signals – ghrelin increases hunger and PYY is thought to increase satiety (fullness). Some patients additionally underwent detailed body composition testing with a whole-body MRI to quantify muscle and fat tissue (a method we have described in previous papers).
We found (Figure 1) that normalization of cortisol levels (from surgical remission) decreased patients’:
- prospective consumption, meaning that patients in remission did not think they could eat as much as patients with active disease. This finding suggests that reduced drive to eat (in addition to numerous metabolic changes), could play a role in the weight loss typically seen in CD patients who have achieved remission. Conversely, an enhanced drive to eat could add to the known metabolic reasons for weight gain seen with active Cushing’s.
- sweet and savory craving, meaning that patients in remission had reduced craving for sweet (e.g. high sugar or carbohydrate foods) and savory (flavorful) foods, suggesting remission may promote the intake of healthr, less sweet, possibly lower calorie foods, and thus could contribute to weight loss after remission. Conversely, these findings suggest that sweet and savory food craving could contribute to the known metabolic reasons for weight gain seen with active Cushing’s.
Unexpectedly, remission did not change hunger, meal-related satisfaction, fullness, or fat craving, despite significant decreases in weight and fat mass. An additional unexpected finding was that ghrelin and PYY, hormones implicated in the regulation of hunger and fullness in the normal population, did not play a role in these appetite meaiesures in patients with active or remitted Cushing’s. Instead, we found that among patients in remission, a higher amount of cortisol in the blood predicted lower meal-related satisfaction and fullness (despite the fact that these measures did not change over time with CD remission). In addition, masses of abdominal fat depots predicted higher hunger and consumption scores in patients in remission.
In conclusion, our findings identify a role for cortisol in food preference, with excess cortisol increasing craving for sweet and savory but not fatty or salty foods. Among patients with Cushing’s in remission, a ‘post-hypercortisolemic’ state, physiologic circulating cortisol concentrations and abdominal fat stores may play a role in food intake by increasing hunger and consumption and decreasing satisfaction and fullness. Continued dysregulation of hunger and satiety signals despite successful treatment could play a role in the persistence of overweight and obesity even in the setting of significant weight loss, and thus the continued cardiovascular and metabolic risk that has been reported in Cushing’s patients despite remission. Our findings demonstrate a role for chronic excess cortisol in promoting behaviors that ensure food intake, such as drive and craving, rather than stimulating sensations of hunger or reducing fullness (as commonly believed), and could help to identify appropriate weight management therapies for patients currently or previously exposed to excess cortisol.
Food-choice behavior in patients with Cushing’s (9)
We then conducted a study to investigate the potential role of brain reward systems in the orchestration of food intake in patients with Cushing’s. In this study, participants chose to view high-calorie food images versus viewing standardized pleasant (e.g., smiling babies), unpleasant (e.g., disfigurement), or neutral (e.g., household objects) images; members of our team originally developed this task for use in cocaine addiction (i.e., evaluating choice for cocaine images). Given data suggesting that, on balance, chronic glucocorticoid exposure is associated with blunted reward processing (10-12), we hypothesized that Cushing’s patients would choose to view fewer food-related and/or fewer pleasant-related images than a sample of healthy controls with similar body mass index (BMI). Moreover, given data suggesting that chronic glucocorticoid exposure drives a metabolic memory that results in long-term cognitive and emotional impairments, even after normalization of cortisol levels, we further hypothesized that such blunted choice, although accentuated in Cushing’s participants with active disease, would also be present in Cushing’s in remission, who would show improved but not normalized reward processing.
We studied 23 patients with Cushing’s (13 with active disease and 10 in remission) compared to 15 BMI-matched healthy controls. On average patients (active and treated) and controls were overweight. Each participant completed two simulated food choice tasks during which, using a computer program, they indicated their objective preference for viewing high calorie food images versus standardized pleasant, unpleasant, or neutral images. We also measured 24 hour urine cortisol and cortisone values in about half of the patients.
Consistent with our hypothesis, we found that participants with active Cushing’s syndrome made fewer food-related choices than participants with Cushing’s syndrome in remission, who in turn made fewer food-related choices than BMI-matched (overweight) controls. Corroborating this finding, higher urine cortisol and cortisone were negatively correlated with food-related choice (in the participants for whom these data were available). In addition, higher food-related choice correlated with higher state (i.e. right now) and trait (i.e. in general) food craving in active Cushing’s patients. Taken together, relative to healthy controls with a similar weight range, Cushing’s patients, particularly those with active disease, displayed a reduced vigor of responding for food rewards that was presumably attributable to cortisol abnormalities.
These findings are consistent with the hypothesis that excess cortisol exposure is associated with blunted reward (here for food) sensitivity. It is possible that active Cushing’s patients have a higher threshold for perceiving food as reinforcing, potentially needing to consume more to achieve the same hedonic effect. An important parallel can be made to addiction literature, whereby reduced drug sensitivity is associated with increased or uncontrolled drug use. Finally, the fact that patients in remission had an intermediate pattern of food choice suggests that prior exposure to excess cortisol has lasting effects on brain reward systems.
More research is needed
This research attempts to understand a few of the many ways excess cortisol exposure can contribute to weight gain. Further studies investigating regulators of appetite and food intake in Cushing’s patients are needed in order to understand why patients with Cushing’s gain weight, and why many patients with treated Cushing’s continue to struggle with weight even after achieving ‘cure’. These studies can use neuroimaging and/or neurochemical approaches in Cushing’s, overweight and normal-weight controls to test for commonalities and/or differences in food choice and its neurobiological underpinnings among these groups. Importantly, prospective studies in patients with Cushing’s are needed to understand the changes each patient experiences over time before and after treatment, and to test whether cortisol-mediated food-choices and preferences have downstream consequences, such as increasing risk for weight gain and/or cardiovascular events in patients despite endocrine remission.
Author: Dr. Eliza Geer, Spring, 2016
Editor’s Note: Eliza B. Geer, MD, endocrinologist, is Medical Director of the Pituitary Care and Research Center and Assistant Professor in Endocrinology and Neurosurgery at Mount Sinai Hospital, New York, New York.
Editor’s Comments: As Editor, I have the privilege of reading these articles before they are are posted. I am on permanent steroid replacement and have recently had to greatly increase my replacement dose due to other medical issues. I found this article to be extremely helpful in attempting to not gain weight while at this increased dose. I seem to wake up every morning and while still in bed, my brain is busy thinking about what sounds yummy to eat that day. Throughout the day, I have tried to pay attention to cravings versus when I am really truly hungry. For me, sometimes a craving will disappear given a bit of time; other times, not so much. Some of the cravings I can delay and others I succomb to, like my Egg McMuffin the other day! I’m also trying to pay attention to portions and trying to pick foods that sound yummy but are healthier or have less calories. Because of the known metabolic effects, I don’t think this strategy will completely stop the weight gain, but I am hoping that by increasing my awareness, it might help some!
References
1. Geer EB, Shen W, Gallagher D, Punyanitya M, Looker HC, Post KD, et al. MRI assessment of lean and adipose tissue distribution in female patients with Cushing’s disease. Clin Endocrinol (Oxf). 2010;73(4):469-75.
2. Geer EB, Shen W, Strohmayer E, Post KD, Freda PU. Body composition and cardiovascular risk markers after remission of Cushing’s disease: a prospective study using whole-body MRI. J Clin Endocrinol Metab. 2012;97(5):1702-11.
3. Hauner H, Schmid P, Pfeiffer EF. Glucocorticoids and insulin promote the differentiation of human adipocyte precursor cells into fat cells. J Clin Endocrinol Metab. 1987;64(4):832-5.
4. Campbell JE, Peckett AJ, D’Souza A M, Hawke TJ, Riddell MC. Adipogenic and lipolytic effects of chronic glucocorticoid exposure. American journal of physiology. Cell physiology. 2011;300(1):C198-209.
5. Slavin BG, Ong JM, Kern PA. Hormonal regulation of hormone-sensitive lipase activity and mRNA levels in isolated rat adipocytes. J lipid res. 1994;35(9):1535-41.
6. Samra JS, Clark ML, Humphreys SM, MacDonald IA, Bannister PA, Frayn KN. Effects of physiological hypercortisolemia on the regulation of lipolysis in subcutaneous adipose tissue. J Clin Endocrinol Metab. 1998;83(2):626-31.
7. Djurhuus CB, Gravholt CH, Nielsen S, Pedersen SB, Moller N, Schmitz O. Additive effects of cortisol and growth hormone on regional and systemic lipolysis in humans. Am J Physiol Endocrinol Metab. 2004;286(3):E488-94.
8. Geer EB, Lalazar Y, Couto LM, Cohen V, Lipton LR, Shi W, Bagiella E, Conwell I, Bederson J, Kostadinov J, Post KD, Freda PU. A prospective study of appetite and food craving in 30 patients with chronic glucocorticoid exposure due to Cushing’s disease. Pituitary, 2015 Oct 23.
9. Moeller SJ, Couto L, Cohen V, Lalazar Y, Makotkine I, Williams N, Yehuda R, Goldstein RZ, Geer EB. Glucocorticoid regulation of food-choice behavior in humans: Evidence from Cushing’s syndrome. In press, Frontiers in Neuroscience, 2016.
10. Ossewaarde, L., Qin, S., Van Marle, H.J., Van Wingen, G.A., Fernandez, G., and Hermans, E.J. (2011). Stress-induced reduction in reward-related prefrontal cortex function. Neuroimage 55, 345-352.
11. Porcelli, A.J., Lewis, A.H., and Delgado, M.R. (2012). Acute stress influences neural circuits of reward processing. Front Neurosci 6, 157.
12. Montoya, E.R., Bos, P.A., Terburg, D., Rosenberger, L.A., and Van Honk, J. (2014). Cortisol administration induces global down-regulation of the brain’s reward circuitry. Psychoneuroendocrinology 47, 31-42.




Sorry, comments are closed for this post.